Is it really necessary to have your wisdom teeth out?
A) Do all wisdom teeth need to be removed?
No, without question a viewpoint that a tooth, just because it’s a wisdom tooth, must be extracted is not justifiable.
Despite some common myths and fallacies (like that they cause tooth crowding), there’s absolutely nothing inherently bad about third molars. Just like any other type of tooth, they can be a valuable part of a person’s dentition (set of teeth).
B) Do impacted wisdom teeth need to be extracted?
It might come as a surprise to you but no, not all impacted wisdom teeth necessarily need to be removed.
It’s certainly possible that a person who has one, or even all four of theirs, will live their entire life without ever experiencing any problems at all.
And in fact, there is a growing consensus (more so in other parts of the world as opposed to the USA) that leaving asymptomatic thirds alone makes the best choice (discussed further below).
Of course, teeth that are, or have the potential to become, problematic should be removed. And this is where your dentist’s experience and judgment come into play. Throughout the remainder of this page, we discuss the signs and issues they consider when making this determination.
What does a dentist consider when evaluating wisdom teeth?
a) Is it impacted? If so, in what way?
One of the primary factors that a dentist will take into consideration when evaluating the need to extract a wisdom tooth is if it is impacted, and if so, its impaction type. Pictures / Diagrams
A tooth’s position in the jaw hints to how troublesome it may be.

Partially-erupted teeth are more likely to be associated with acute flare-ups (swelling, pain) than full-bony impactions.
- Overall, full bony impactions (a situation where the tooth is fully encased in the jawbone) are the type of impaction that’s least likely to cause problems.
(The types of problems most associated with full-bony impactions would typically fall along the lines of cyst or tumor formation Learn more., or the cause of damage to a neighboring tooth Learn when & how.. However, these are comparatively lower frequency events with wisdom teeth (Breeze).)
- Partially erupted teeth (the situation where just a portion of the tooth sticks through the gums) are the type most likely to become problematic.
(It’s their connection with the oral cavity, and thus the bacteria it harbors, that places these teeth at greater risk for complications, especially pericoronitis (infection) Details or the formation of periodontal disease (gum disease) Details and/or tooth decay. Details These are all relatively common occurrences with wisdom teeth (Breeze).)
b) Is the tooth really impacted?
At least some wisdom teeth that have been classified as impactions probably aren’t. That’s because when they were evaluated the full time frame associated with the normal eruption process of third molars wasn’t fully kept in mind.
Checklist: Do your wisdom teeth really need to be extracted?
- Is there any pathology associated with the teeth?
- What age are you?
- Are your teeth truly impacted or still erupting?
- Is a wait-and-see approach appropriate? (What monitoring is needed? How long should the teeth be given?)
- If impacted (full vs. partial), what level of risk is posed?
- What dental risks and concerns does removal involve?
- What health issues are posed if surgery is performed?
- What is your preference?
Print out. Take notes as you read along.
- A typical time frame for third molars to come in is between the ages of 16 and 25 years.
(Hupp’s textbook of oral surgery states: “The average age for completion of the eruption of the third molar is age 20 years, although eruption may continue in some patients until age 25 years.”)
- That means that until the end of this age range, it’s at least theoretically possible that the tooth being evaluated is still in the process of erupting and simply has not reached its final positioning yet.
- That’s not to say that in some, or even many cases, that the current orientation of the tooth makes it painfully obvious that that will never happen (especially horizontal and distal impactions Pictures / Diagrams). But at the same time, with relatively normally oriented teeth it might be debated if the term “impacted” really applies.
Using a wait-and-see approach with third molars.
In those cases where available jaw space and the tooth’s alignment appear to fall relatively well within normal limits (especially vertical or mesial orientations Pictures / Diagrams), then quite possibly the tooth should simply be given more time to progress with its eruption process.
Then, at an age lying closer to the end of the normal eruption time frame, if it appears that the tooth really won’t come in properly, it can still be extracted within that time window typically considered best for extracting wisdom teeth (the upper end of this range is age 24 When to extract wisdom teeth).

Mesially inclined teeth may still erupt properly.
There’s evidence that supports a wait-and-see approach with wisdom teeth.
Of these impacted teeth (whose forward tilt ranged between 5 and 30 degrees), 37% managed to successfully erupt (come into position fully) and 15% accomplished partial eruption.
c) The patient’s age must be factored in.
When making a decision about what to do about an impacted wisdom tooth, it’s important to consider the patient’s age.
Considerations.
There is no question; comparatively younger patients tend to experience fewer complications Common complications. with third molar surgery than older adults.
Because of this, for those 35 years of age and beyond, if an impacted wisdom tooth exists (especially a full bony impaction) and it’s not causing problems and shows no evidence of associated pathology, a decision is frequently made to just leave it alone.
d) Any retained wisdom teeth should be monitored regularly.
Over time, a wisdom tooth’s status may change. This includes both the formation of pathology (cysts, tumors, decay), or a change in its positioning (a full-bony configuration may transform into a less predictable partially-erupted one).
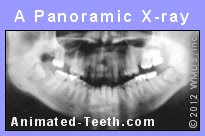
Panoramic x-rays are usually used to evaluate 3rd molars.
X-ray examination will be required.
▲ Section references – Hupp
e) Other complications and risks must be considered.
1) All surgery involves risk.
It’s important to keep in mind that all types of surgery, including oral surgery, contain some inherent risk, no matter how minor.
For this reason, wisdom teeth should only be extracted in those cases where a reasonable case for their removal can be made. (See our page: Reasons to extract wisdom teeth.)
2) The patient’s health status must be considered.
The status of a person’s health may contraindicate having an extraction. Considerations include underlying systemic disease and factors that may complicate or interfere with the healing process [diabetes, hepatic (liver) disease, blood disorders, renal (kidney) disease, steroid therapy, contraceptive medications, immunosuppression, and malnutrition].
In some cases, it may be possible to remove the wisdom tooth after the patient’s medical issues have been resolved.
3) Is there potential for damaging neighboring teeth or anatomical structures?
In some cases, the surgical procedure associated with accessing and removing an impacted wisdom tooth might be such that it’s possible that nearby teeth or anatomical structures may be damaged.
As an example, lower wisdom teeth often lie in close relationship to the mandibular nerve. Trauma to this nerve can cause postoperative lip numbness (termed paresthesia), which may be permanent.
In other cases, the neighboring second molar, surrounding bone tissue or even the jawbone itself might be damaged, fractured or otherwise compromised during the procedure.
f) Recommendations of health organizations about wisdom tooth removal.
A number of agencies and associations worldwide have evaluated the issue of prophylactically removing asymptomatic third molars.
Most of them have taken a stance that extraction is not indicated unless the teeth have created or become associated with a pathological condition. (American Public Health Association – 2008, British National Institute for Clinical Excellence – 2000, Belgian Health Care Knowledge Centre – 2012, Scottish National Clinical Guideline – 1999, Regional Health Technology Assessment Centre [Sweden] – 2011). (Boughner)
In contrast to this opinion, the American Association of Oral and Maxillofacial Surgeons (AAOMS) in a White Paper statement (2011) projects the stance that all third molars are inherently prone to disease and therefore make reasonable candidates for removal. Other publications issued by the AAOMS suggest that this assessment even includes those teeth that have come into a normal, upright position. (Boughner)
▲ Section references – Boughner
Page references sources:
Boughner J. Maintaining Perspective on Third Molar Extraction.
Breeze J, et al. Are soldiers at increased risk of their molar symptoms when on operational tour in Iraq? A prospective cohort study.
Hattab, F. Positional changes and eruption of impacted mandibular third molars in young adults. A radiographic 4-year follow-up study.
Hupp J, et al. Contemporary Oral and Maxillofacial Surgery. Chapter: Principles of Management of Impacted Teeth.
All reference sources for topic Wisdom Teeth.