Dental implant vs. root canal, which makes the better choice?
Using dental implants as a way to replace missing teeth has gained widespread acceptance over the last few decades. And dental patients who are aware of the success of this technique may wonder:
- “If my tooth is so damaged that it needs root canal treatment, why not just have it extracted and get a dental implant placed instead?”
We agree, this is a very logical question to have.
What needs to be considered when making this decision?
As the remainder of this page outlines, when deciding between the two there are some fundamental issues that must be weighed. They include:
- How might the specifics of your case affect the expected rates?
- How does the dentist’s level of training tend to affect case success?
- Case-specific treatment challenges.
- Patient’s needs and preferences.
- We cover this topic as a separate issue and you can find our discussion here: Cost-effectiveness calculations for implants vs. root canal.
1) Dental implants vs. root canal treatment – Success rates.
Definitively proving which of these treatment options creates a better outcome is difficult. After all, if one of the procedures has been performed, it’s impossible to know what the outcome of the other would have been.
However, if the success rate of each is considered independently, they can be compared and you can come up with an answer, at least in general terms. And, for the most part, dental research tends to show that both treatment approaches can make an excellent choice.
Dental implant vs. root canal treatment.
Dental research.
Study #1 –
 (Blicher 2008)
(Blicher 2008)- Evaluated the survival rate of teeth that had received root canal treatment.
- Evaluated the success or failure of dental implant placement.
- The success rate for root canal treatment ranged between 92 and 97% (over a time frame of four to eight years)
- The success rate for dental implants ranged between 95 and 99% (over a time frame of two to sixteen years).
These results suggest that the overall success rate of either treatment approach is fairly similar, although slightly favoring dental implants.
Study #2 –
Title: “For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations?” (Iqbal 2007)
(Iqbal 2007)
This paper, which was also a literature review, took into consideration 55 research studies that had evaluated dental implants and 13 that evaluated root canal therapy. It came to the conclusion that:
- No significant differences in survival rates existed between the two treatment approaches (root canal vs. implants).
The paper continued by stating that a decision between the two should be based on factors other than just the statistical analysis of predicted treatment outcome (success rate). (See lower on this page for an outline of factors that should be considered.)
Study #3 –
Title: “Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review.” (Torabinejad 2007)
(Torabinejad 2007)
This third dental literature review conducted during the same time frame as those above concurred with their findings.
- It determined a 97% long-term survival rate for either an extraction/implant or root canal/restore-tooth treatment approach.
- The paper went further in stating that either of these approaches could be expected to provide a superior outcome to extracting the tooth and replacing it with a dental bridge.
Conclusions:
Together, the findings of all three of these reviews suggest that either treatment option (endodontic therapy or implant placement) can make an excellent choice. However, this assumes that a proper standard of care has been practiced (see our next section).
And while there may be specific circumstances why one or the other might make the much better choice in any one situation (see checklist below), as a general rule neither has been universally proven to provide a significant advantage or be the preferred approach.
Root canal vs. implant placement: Which treatment approach do most people prefer?
The Torabinejad (2007) paper mentioned above contains a section that discusses this subject. And it cites a number of sources from which the following statistics are taken.
- 90% of patients would choose to have root canal treatment again. 88% of patients who have had an implant placed would choose that approach again.
- Patient satisfaction ratings for both techniques exceed 90%.
In light of those numbers, it seems safe to say that neither method holds an edge in terms of patient experience or outcome.
▲ Section references – Torabinejad
2) Maximizing your chances for a successful outcome.
a) Pick the proper clinician.
It’s important to understand that different dentists have different levels of training. And with any case, but especially challenging ones, the knowledge and expertise of the clinician can significantly affect the outcome of the work that’s been performed.
i) Clinician success rates for root canal treatment.
A study by Alley (2004) found that 98% of routine cases treated by endodontists (root canal specialists) were successful vs. 90% for those treated by general dentists.
[Beyond just increased training and experience, most endodontists incorporate equipment into their practice that general dentists typically just don’t have. This includes a surgical operating microscope.
These instruments assist the clinician in identifying any minute root canals that might exist and this aids clinical results. After all, even the most talented general dentist can’t successfully treat canals they can’t locate.]
ii) Clinician success rates for implants.
Unlike the field of endodontics (root canals) that’s been taught for decades, implantology (at least the way it’s practiced now) is a much newer field. It’s only been since the 1990’s that it’s been a regular part of the curriculum of dental schools.
Specialist vs. general dentist.
Early on, dental implants (at least the ones evaluated by the earliest longevity studies) were typically placed by dentists having a “specialists” level of training (either in oral surgery or periodontology). In comparison, nowadays it’s routine for implants to be placed by general practitioners.
It could be debated that collectively, the work performed by general practitioners doesn’t equate to the high standard of care typically practiced by specialists.
- A hint of this phenomenon might be apparent in data coming from Australia. There, the largest category of implant-related claims against dentists (24%) is founded on errors associated with inappropriate diagnosis and case selection (Cohn 2005).
This is the type of error that might be more likely made by a less rigorously trained practitioner.
- In an overview of the topic of placing implants vs. salvaging teeth via performing root canal treatment, Parirokh (2015) states that the operating practitioner’s level of experience plays a vital role in implant success: “In hands of an inexperienced dentist, the survival rate drops to 73%, compared to 95.5% survival rate of implants placed by specialists.”
▲ Section references – Cohn, Parirokh
iii) Be a consumer. Ask your dentist questions.
We’re not trying to suggest that a general practitioner can’t provide quality implant and endodontic services because that statement would not be true.
But what we are suggesting is that before accepting a recommended treatment plan, be a consumer first. Quiz your dentist about their experience in providing the proposed treatment.
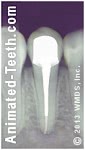
A tooth that has had root canal and a crown placed.
b) With root canal, you must commit to complete treatment to reap the highest success rate.
3) If the success rates of both are similar, what other factors need to be considered?
The fact that both root canal treatment and dental implant placement have high and comparable success rates suggests that the decision between the two will need to hinge on other factors.
Checklist of issues:
Here’s a list of factors and issues your dentist will consider when trying to come to a conclusion about what treatment approach makes the best plan for you. If you think possibly any of them apply to your situation, you should make a point of discussing them with your dentist.
a) How important is it to you to retain your natural teeth?
Generally speaking, the primary emphasis of modern dentistry is helping the patient to keep their natural teeth. And for this reason, when evaluating the question of extraction and implant placement vs. “saving” the tooth by way of performing root canal therapy, most dentists will likely lean toward the latter.
This, of course, presumes that performing the work, including rebuilding the tooth after its endodontic therapy has been completed, is expected to be routine (see our next section).
Advantages of “saving” your tooth.
While not always so significant, there are some reasons why retaining a natural tooth has advantages over implant placement.
- A study of patients by Gatten (2011) reported that some people who receive implants state that their artificial tooth “feels different” than their natural ones, although growing accustom to this difference over time seems to be the norm.
- At least a part of the above effect has to do with the fact that the ligament that binds a tooth in its socket provides sensory feedback. And beyond just how an individual tooth might feel, this feedback also helps you in controlling your jaw’s movements (direction, speed, amount of force) and helps you to prevent problems such as overloading your jaw joint.
We won’t pretend that this is a big issue when just a single tooth has been replaced. But if enough teeth have been sacrificed, this loss of sensation might become significant.
- Implants osseointegrate (fuse) with the jawbone, which means that future orthodontic movement of that tooth (i.e. having braces) is not possible.
- There can be negative psychological effects associated with tooth loss. Generally speaking, people tend to prefer the idea of keeping their natural dentition (teeth).
b) Clinical issues:
i) Can the tooth’s root canal therapy be completed successfully?
Obviously, if the dentist expects that there will be significant challenges to being able to successfully complete the tooth’s endodontic therapy, placing an implant will likely make the better choice.
a) Initial tooth treatment.
As mentioned above, routine conventional root canal therapy can be expected to provide a predictable and lasting outcome. Especially when the work has been performed to a high standard of care (see above).
Reasons not to treat.
Even so, circumstances may exist that will ultimately result in treatment failure. This can include significant cracks within the tooth or its root(s). Or internal tooth anatomy that’s difficult, or even impossible, to adequately treat.
If the dentist performing the work is able to identify such problems, a recommendation of extraction and implant placement can be expected.
b) Teeth requiring retreatment.
Some patients face the decision of “saving” or “pulling” their tooth at that point when it’s discovered that its original root canal treatment has failed.
Retreatment is less predictable.
While the success rate of a tooth’s initial endodontic therapy can be quite high (90 to 98%, see above), with less than ideal cases (like retreatment) this number begins to fall. And especially in cases where surgical retreatment is required (“apical” surgery), the predictability of the procedure’s outcome drops even further.
When it comes to retreatment, if it can be performed conventionally (through an opening created in the tooth) doing so may still make the best choice. But if surgical intervention is required (accessing the tooth’s root via a gum incision and bone removal), extraction and the placement of an implant may make the better choice. (DiMatteo 2008)
c) Considerations associated with COVID-19.
With a tooth’s initial therapy or retreatment, the recommendation that your dentist makes may be influenced by practice-changing events such as the COVID-19 pandemic.
In the pre-pandemic era, any level of outcome uncertainty associated with comparatively lower-prognosis endodontic cases may have been considered acceptable. But nowadays, since additional appointments will be needed to manage or correct complication and failure issues (which might be associated with increased risk for exposure to pathogens), choosing the solution that has the greatest level of outcome predictability (possibly extraction and dental implant placement) may be considered significantly advantageous for all involved.
ii) What will it take to rebuild the tooth?
Teeth that require endodontic therapy have frequently experienced some type of catastrophic event. This could include fracture or advanced tooth decay. If so, the question then becomes how involved will rebuilding it be?
Doing so may be fairly routine (such as dental crown and post placement). But in some cases, additional procedures may be required too. Or conditions may be so deteriorated that rebuilding the tooth is impractical or ill-advised.
Complications with severely damaged teeth.
Dentists have specific rules they must follow when restoring teeth. With broken-down ones, one of them is that the restoration placed must not extend so far underneath the gum line that it’s close to the underlying bone. If this rule is broken, gum health around the tooth will be a perpetual problem, likely affecting the neighboring teeth too.
Additional procedures.
A surgical procedure, termed crown lengthening, can be performed to remedy this situation. But doing so removes some of the bone that supports the tooth (and usually from around the adjacent teeth too). Beyond that disadvantage, there’s also the issue of the additional time (including healing time) and expense of performing this procedure.
Teeth that are easily rebuilt can make excellent candidates for being “saved.” But if a complication exists, extraction and the placement of a dental implant may prove to be the more prudent choice.
iii) Does the tooth have good gum health?
If the tooth in question has advanced periodontal (gum) disease, extracting it and placing an implant likely makes the better choice.
That’s not to say that patients who have generalized poor gum health make suitable candidates for implant placement. But clearly, if a tooth’s compromised status cannot be corrected, “saving” it by performing root canal treatment makes no sense.
iv) What will be required to place an implant?
Just as natural teeth may require additional procedures to successfully repair them, dental implant placement may require performing additional procedures too.
The patient’s jawbone may require tissue grafting or bone augmentation (such as a sinus lift procedure). If so, the case will involve added expense and time (including healing time). In comparison, retaining the existing tooth may make a more attractive choice.
v) Esthetic considerations.
Especially when a front tooth is the one being treated, factors involving the appearance of the procedure’s final outcome will be a prime consideration.
a) Challenges with teeth that receive root canal treatment.
For the most part, improving the appearance of a tooth that has had root canal treatment is usually a fairly straightforward task. And if needed, even substantial improvements can be made with cases where a dental crown is placed as the final restoration.
But in some cases, original factors like exceptionally poor tooth alignment may make creating the ideal esthetic outcome virtually impossible. In comparison, tooth extraction and replacement with an implant may be able to make this type of alignment change quite readily.
b) Challenges with dental implants.
Implant positioning.
When placing an implant, the dentist must adhere to rules dictated by characteristics of the jawbone (such as its shape, bone quality and position of nearby anatomical structures).
And in some cases, having to follow these guidelines may interfere with placing the implant in a position that’s most ideal for esthetic purposes.
Implant / gum line concerns.
Another issue involves the region where the implant’s crown meets the gum line. In some cases, it can be difficult for the dentist to make this junction look totally natural.
This consideration may make “saving” the tooth the better choice for people who display this area prominently when they smile (like people who have a “skin grin”).
Despite the above considerations, we should point out that Torabinejad (2007) states that dental implant literature generally reports very high levels of patient satisfaction when it comes to the esthetic outcome of implant cases.
c) Ask your dentist questions before your treatment begins.
You can expect that your dentist will be quite aware of the issues we have mentioned above. But what they might consider a minor compromise in appearance may not be acceptable to you.
As a way of avoiding a disappointing surprise, if the issue of cosmetics is a major consideration for you, ask questions about the expected esthetic outcome of your case before you decide on a treatment approach.
vi) Is having surgery a problem for you?
Extracting a tooth and placing a dental implant are both surgical procedures whereas having root canal treatment and subsequently rebuilding the tooth is not. (Conventional endodontic therapy involves performing the tooth’s work through an opening made on its backside or chewing surface.)
Patients who have a fear of surgery or are uninterested in experiencing its potential side effects will prefer the approach where their tooth is retained.
vii) How much post-op discomfort is involved?
A study by Torabinejad (2014) quizzed patients that had opted for either root canal treatment and rebuilding their tooth, or extraction and implant placement. Both groups reported that the level of postoperative pain that they experienced was just minimal.
Simply due to the nature of these respective treatment processes, for the root canal group the highest incidence of pain was reported on the day following their endodontic therapy. For the implant group, maximum discomfort was reported at the end of the week following their implant placement.
▲ Section references – Torabinejad
viii) Lifestyle considerations.
With both procedures, questions should be asked and answered about issues that may disrupt the person’s normal lifestyle.
This might include issues such as the expected level of post-procedure discomfort or how post-op numbness, swelling, oral dressings, etc… might affect eating, speaking, appearance, etc…
c) What time frame is needed to complete treatment?
A patient’s choice of implant vs. root canal might be swayed by the total amount of time (procedure and healing) that each procedure requires.
Blicher (2008) cites a 2001 survey that reported that:
- Performing root canal treatment and then placing a dental crown typically requires 4.5 hours of appointment time, broken up into six visits, over a time span of three months.
- Restoring a tooth’s space with a dental implant typically takes 5.5 hours of appointment time, divided among ten visits, over a time span of 9.5 months.
So while the total amount of procedure time is similar for both, the time span over which it takes to complete treatment is roughly three times longer with implants. This might be of prime importance when the functional and esthetic inconveniences of your case are considered.
▲ Section references – Blicher
Your mileage may vary.
Only your dentist is in a position to know what time frame will be needed for your case. For example, some treatment plans will require additional procedures.
- Root canal cases – If the tooth is badly broken down (portions of it don’t even rise above the gum line), crown lengthening may be indicated. Or, if the tooth has complications associated with periodontal disease, gum surgery will be required.
With either procedure, additional weeks of healing time will be needed (6 or more).
- Implant cases – If the quantity or quality of the gum tissue or bone in the region of the implant site is found to be deficient, some type of surgical procedure (augmentation, grafting) will be needed.
Afterward, some additional months of healing are usually required.
d) Do you grind your teeth?
A habit of tooth clenching or grinding (referred to as bruxism by dentists) may complicate the placement or longevity of dental implants. If this activity can’t be controlled, root canal treatment may make a better choice.
e) Medical considerations.
Health issues can affect the outcome of implant therapy. For example, root canal treatment may make a more predictable choice for patients who have uncontrolled (or poorly controlled) diabetes or are smokers. (More details.)
f) Treatment costs.
We’ve chosen to explore the issue of relative cost and cost-effectiveness for root canal therapy vs. implant placement separately. You can find this discussion on this page.
Traditionally dental insurance policies have been more likely to provide benefits for root canal treatment (and crown placement) as opposed to dental implants. Where both are actually covered, the level of benefits paid for each frequently differs. Any of these discrepancies may make choosing one procedure over the other quite easy.
Page references sources:
Alley B, et al. A comparison of survival of teeth following endodontic treatment performed by general dentists or by specialists.
Blicher B, et al. Endosseous implants versus nonsurgical root canal therapy: a systematic review of the literature.
Cohn S. Treatment choices for negative outcomes with non-surgical root canal treatment: non-surgical retreatment vs. surgical retreatment vs. implants.
Gatten D, et al. Quality of life of endodontically treated versus implant treated patients: a university-based qualitative research study.
Iqbal M, et al. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations?
Parirokh M, et al. Choice of Treatment Plan Based on Root Canal Therapy versus Extraction and Implant Placement: a Mini-Review.
Torabinejad M, et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review.
Torabinejad M, et al. Degree of patient pain, complications, and satisfaction after root canal treatment or a single implant: a preliminary prospective investigation.
All reference sources for topic Dental Implants.
Comments.
This section contains comments submitted in previous years. Many have been edited so to limit their scope to subjects discussed on this page.
Comment –
Implant after root canal.
Hello. My question is what if I want to remove that one tooth that is bothering me? I have gum disease and lost bone where the bone should have been in my mouth. so down the road, I was thinking of getting a dental implant to replace the root canal later, leaving no tooth in the area of the root canal failure. so if I get a dental implant while having gum disease is it worth the time to replace the one tooth with an implanted tooth?
klr
Reply –
Usually, the placement of implants is contraindicated in the presence of periodontitis (gum disease). (The presence of the gum disease may interfere with the healing process of the implant.)
Also, your gum disease may lead to the loss of other teeth. If so, in terms of the larger picture of rebuilding your mouth, having an implant in the location of your failed root canal tooth may or may not be a part of the plan that’s needed.
Usually the better plan involves: Treating the patient’s emergency situations first. Then treating their gum condition. Then completing their treatment by rebuilding teeth and replacing missing ones.
Staff Dentist
Comment –
Mistake made by dentist
While doing tooth prep for crown and placing post in a root canalled tooth, my dentist perforated the root with the post. Now being sent to specialist and am considering an implant instead. Should dentist cover cost of error?
CKP
Reply –
Generally, a perforation would considered an “iatrogenic” event, meaning it stems from the actions of the dentist. However, iatrogenic complications don’t always stem from malpractice. In some cases, what has resulted may have been due to a condition/situation that was unforeseeable.
In the case of a perforation being created during post placement, if the root had some uncharacteristic anatomical shape or properties that couldn’t be visualized on the type of x-rays dentists routinely take, that would be one thing.
If the dentist instead was overly aggressive in the way they created the post space, or poorly planned the procedure, would be another. (That page gives some examples.)
When asked, your specialist (endodontist?) has an obligation to provide you with a truthful opinion about how they interpret your case. They also have an obligation to provide you with an opinion about the anticipated success of the planned repair, and how that anticipated success might compare with other possible alternatives (such as extraction and implant placement).
As a provider, your dentist has an obligation to perform your procedure (skill level, case planning) at a level that’s commensurate with that that would be provided by other general dentists in your area. Your endodontist would be well seated to provide an opinion on that issue.
Staff Dentist